Day 1 :
Keynote Forum
Julia Sanders
Cardiff University, UK
Keynote: Supporting women to achieve healthy weight gain in pregnancy

Biography:
Julia Sanders has combined teaching, research and midwifery practice for over 25 years and has extensive experience in the design and delivery of complex research studies into maternity care. Her current methodologies include randomised trials and the use of routine health data to answer research questions. Julia is currently leading the UKs largest study comparing outcomes for mothers and babies following waterbirth and birth on land and has an interest in developing further work around maternal weight gain in pregnancy.
Abstract:
Background: Excess antenatal weight gain is associated with pregnancy complications and longer term maternal obesity. Although international guidelines on antenatal weight gain exist, women have reported information to be inadequate. This presentation will explore the current evidence base in relation to gestational weight gain and present the results of a UK based study.
Aim: The PRAM study assessed the feasibility and acceptability of incorporating an individualised weight chart and midwife support using a motivational interviewing-informed approach, into antenatal care.
Method: Pregnant women were recruited by community midwives and provided with personalised weight (based on their BMI) to record pregnancy weight gain against a plotted range based on the IOM guidelines. Participating midwives were trained in a motivational interviewing-informed approach to discussing weight. Participants were followed up postbirth and weight charts reviewed. Participant qualitative interviews and midwife focus groups were conducted.
Results: Fifty two women were recruited across all BMI categories. Weight charts were obtained from 33 (63.5%) participants’ maternity notes; 29 participants (87.8%) had monitored weight ≥10 times throughout pregnancy and 4 participants (12.1%) had monitored their weight 1 to 9 times. Gestational weight gain was obtained for 41 participants (78.8%) and compared to IOM recommended parameters. Of these, 11 participants (27%) were in range, 19 (36.5%) were above and 11 (21.2%) below recommended parameters. Interviews / focus groups with participants and midwives revealed that the weight charts were generally acceptable to participants, but that midwives did not engage participants in discussions about their weight as part of antenatal care.
Conclusions: Monitoring of gestational weight gain in pregnancy is generally acceptable to women and could be incorporated into an antenatal weight management intervention. However, given current evidence careful consideration now needs to be given to establishing healthy weight ranges for pregnancy and the development of effective tested complex interventions for women.
Keynote Forum
Sarah Chitongo
Middlesex University, UK
Keynote: Midwives` competencies in caring for high risk women: An exploration of midwives` care to women from Black Minority Ethnic (BME) Groups on delivery suite High Dependency Units (HDU)

Biography:
Sarah Chitongo is a Nurse and Midwife with 16 years of experience in all areas of Midwifery. She is also an experienced Senior Manager who left the National Health Service (NHS) as a Deputy Head of Midwifery. She has set up a High Dependency Unit (HDU) on a delivery suite. The aim of the HDU was to offer women and their families a consistently high level of individual, medical, and psychological care, delivered by staff who understood the physiology, pathology, psychological and cultural needs of BME obstetric groups and the wider community. There was initial anxiety on the part of midwives around the mechanization of care, but competence and confidence was developed through an informal structure that she developed. She is an ambitious manager who has built a reputation developing and motivating staff. The management style focuses on three main things; innovation, quality and staff. She has excellent leadership, communication and interpersonal skills with the ability to inspire confidence and build strong stakeholder relationships to ensure that the curriculum is at the forefront of knowledge and reflects the latest research insights and materials. Further roles within current position include generating and presenting annual management review reports as well as providing consultancy for academics within the department in relation to midwifery education.
Abstract:
The Black Minority Ethnic (BME) population has increased significantly over the course of the last three decades. They have more prevalent pre-existing medical conditions and have worse health outcomes. With the increase in births from this group, it is inevitable that midwives’ are increasingly caring for these women in High Dependency Units (HDU) on delivery suites and engage in a meaningful way with midwives’ in understanding their experiences of HDU care on delivery suite. Little is known about midwives’ competencies and experiences in caring for this group. Hence, we need to identify barriers that affect high dependency provision to BME patients. A mixed study using surveys to London based Trusts. Knowledge from this work will contribute to guidance on standardization of this area and identify areas of improvement. It will also reduce the fragmented care provision and encourage responsiveness to individual, family and cultural needs. Encourage services is to be organized more seamlessly to ensure ethnic minorities receive appropriate individualised maternity care.
- Women’s Health | Midwifery | Midwifery Practice and Education | Maternal and Child Health
Location: Spessart

Chair
Elinor Jenkins
Isle of Wight NHS Trust, UK
Session Introduction
Faezeh Safari
King's College London - Guy's Campus, UK
Title: A qualitative study of women's lived experience after deinfibulation in the UK
Time : 10:55-11:15

Biography:
Faezeh Safari is a Senior Midwife at King's College London-Guy’s and St. Thomas’ Hospital, NHS Trust, London since 2003. She is currently practicing as a Community and Birth Centre Midwife. She has completed her BSc in Midwifery at Survey University in Iran in 1999. She has completed her MSc in Advancing Women’s Health Care at King’s College London University which led her to research and publication on women’s experience of de-infibulation in the UK. She is a Member of the Royal College of Midwifery in the United Kingdom. She also worked as a Research Midwife in the Department of Maternal and Fetal Research Unit at King’s College London. She is a strong advocate of midwives and natural childbirth. She is a mentor and sign off mentor for clinical practice of student midwives.
Abstract:
Geraldine McLoughlin
University College Cork, Ireland
Title: ‘Wearing the Mask of Motherhood’: The experience of maternal attachment using interpretative phenomenological analysis
Time : 11:15-11:35

Biography:
Geraldine Mc Loughlin is a Midwife Lecturer and BSc (Hons) Midwifery Programme Co-Ordinator in the School of Nursing and Midwifery at University College Cork. Her PhD in Education explored Maternal Fetal/Infant Attachment during the transition to new motherhood using interpretative phenomenological analysis. She teaches modules across undergraduate and postgraduate midwifery and nursing. She also collaborates with continuing professional development in the acute Maternity hospital setting facilitating multidisciplinary training in PROMPT Obstetric Emergency Programmes and Neonatal Resuscitation Programmes. She has extensive senior clinical experience in all aspects of midwifery care in both the community facilitating home births and water birth and in the acute obstetric setting. She is experienced in quantitative and qualitative research methodologies particularly interpretive phenomenological analysis. Other research interests include psychological health during pregnancy and early motherhood, transition to parenthood, maternal morbidity and mortalities associated with childbirth, and organisational management of care.
Abstract:
Becoming a mother is an intense experience which sets the foundation for future interactions and relationships for both mother and baby. Researchers have theorized that maternal infant attachment begins during the antenatal period and continues on through the postnatal period, though the reality of the experience for the mother remains largely unexplored. There are many variables, complexities and concepts that influence the maternal foetal/infant attachment relationship. Accordingly, this study examined how the concepts of transition to motherhood and identity influence a mother’s experience of the attachment relationship during pregnancy and with her baby. Understanding these experiences has implications for practice and is relevant to the particular needs of the women, babies and families in our care and society. This three-phase project adopts a phenomenological approach where semi-structured interviews were used to collect data from nine women during pregnancy at approximately 35 week’s gestation and at six and twelve weeks postnatal. Interpretative phenomenological analysis was utilized to synthesize themes. The super ordinate theme which emerged from the data during pregnancy was attachment relationship with the unborn baby and following birth: attachment interrupted and getting to know you emerged from the women’s narratives. Following on from this, at twelve weeks postnatal the women had achieved a new understanding of their experience as reflected in the super ordinate themes: ‘I have finally arrived’, and ‘Identity-wearing the mask of motherhood’. The longitudinal dimensions of the study enabled narratives to be collected valuing the unique perspectives of the participants and respectful of their lived experience, revealing ways in which the transition to motherhood and the experience of attachment from the maternal perspective is socially constructed and personally experienced. The epistemological and ontological perspectives led women to challenge assumptions around mothering which they may have previously held, which influenced their expectations and rendered experiences which did not conform to idealised notions of motherhood, difficult to voice or express. The women’s narratives of their subjective experience convey the overwhelming nature of motherhood and the multifaceted phenomena that influence the attachment relationship. This study provides an insight into the experience of the transition to motherhood, the development of the attachment relationship of first-time mothers and how maternal identities are revealed by the narratives they convey. It also highlights the complexity of the maternal foetal/infant attachment. Finally, implications for education, research and practice are explored and elaborated.
Soheyl Asadsangabi
Vanderbilt University Medical Center, USA
Title: Women’s health and cultural diversity: What does it mean?

Biography:
Soheyl Asadsangabi has completed her DNP as a Midwife at Vanderbilt University. She has been practicing midwifery since 2004 in private and academic settings. As a woman from another culture and a clinician who provides care for a diverse population, her focus is on cross cultural women’s health care. She is currently an Assistant Professor at Vanderbilt School of Medicine.
Abstract:
By 2013, Western countries received roughly 130 million immigrants, with women consisting of more than half the immigrant population. This demographic change highlights the importance of cultural sensitivity and its role in clinical practice. The impact of cultural diversity in the delivery of quality health care is undeniable. Sociocultural differences, e.g., ethnicity, race and language proficiency, are just a few factors to consider. Furthermore, these differences directly influence a woman’s perspective, behavior, belief and value in current multicultural societies. A true understanding of a woman’s cultural differences is required to establish effective clinician-patient communication and to improve quality of care. Through applied and innovative understanding, it is possible to continue the integration of diversity in women’s health management and establish standards of care for this vulnerable population. Standards to consider may include availability of personalized care, cultural respect, informed consent in medical decision-making and medical procedures, understanding of sexual orientation, use of interpretive services, and regard for all birth rituals and faith-based concerns. The purpose of this presentation is to: Define cultural diversity in women’s health; Identify obstacles in cross-cultural care; Introduce sensitive models to care for women from other cultures
Sevil Hakimi
Tabriz University of medical science, Iran
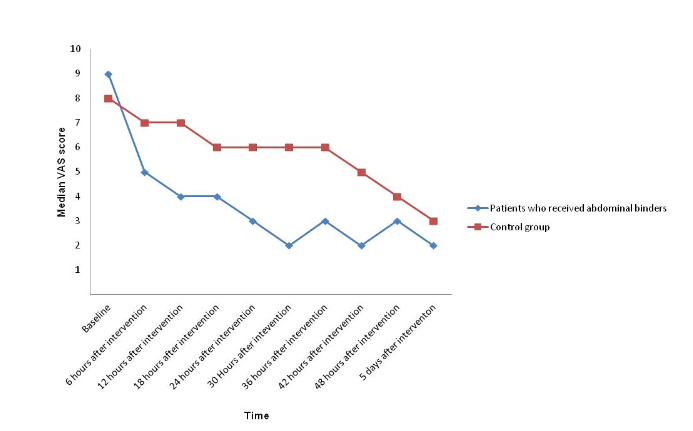
Title: Randomized controlled trial of abdominal binders for postoperative pain, distress, and blood loss after cesarean delivery

Biography:
Abstract:
Objective: To assess the effect of using abdominal binders on pain, distress, and postpartum hemorrhage after cesarean delivery.
Methods: The present prospective randomized controlled trial enrolled patients undergoing non-emergency cesarean deliveries in Golestan Province, Iran. Patients were randomized in a 1:1 ratio by blocks of four or six to a control group or to use an abdominal binder after delivery; all patients received routine care. The primary outcomes were visual analog scale-assessed pain, symptom distress scale (SDS)-assessed distress and hemoglobin and hematocrit levels. Participants and researchers were masked to treatment assignments until after cesarean delivery and data analysis was unmasked; intention-to-treat analyses were performed.
Results: There were 89 patients enrolled in each group, with no differences in baseline pain scores, SDS scores and hemoglobin and hematocrit levels between the groups (all P>0.05). Pain and SDS scores were lower in the binder group at all post-baseline time points compared with the control group (all P<0.001). Hemoglobin and hematocrit levels were higher among patients who received binders 36 hours after baseline (both P<0.001). There was one patient who experienced hemorrhage in the binders group and one patient requested removal of their binder.
Conclusions: Patients who received abdominal binders reported less pain, lower SDS scores and higher hemoglobin and hematocrit levels following cesarean delivery.
Indrayani
Akademi Kebidanan Bina Husada, Indonesia
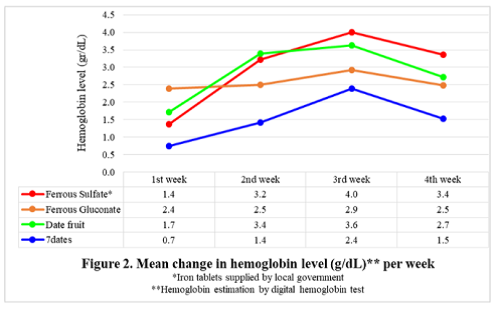
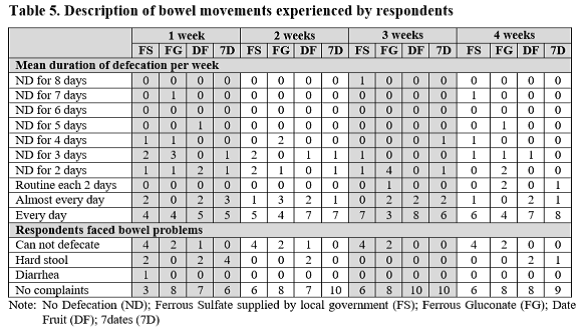
Title: Effects of date fruit and 7dates consumption on hemoglobin level and bowel movement

Biography:
Indrayani is a Midwife with several working experiences as a Nurse of Public Health Center, Midwife Practitioner, Midwife Lecturer, Researcher, and Writer. Her research interests include “Midwives in communities, midwifery education, and maternal mortality particularly postpartum haemorrhage”. Her job has led her to work with several collaborative partners such as the Ministry of Health, government and non-government institutions, association and broader community of midwives. She has published four books on midwifery and more than 19 papers of presiding and journals both nationally and internationally.
Abstract:
Statement of the Problem: Iron supplement program as an approach to overcome anemia gives positive impacts but still under expectations, even considered a failure. Side effect of iron supplement such as constipation causes disobedience. This study was designed to examine haemoglobin level and bowel movement differences resulted from iron supplement of government program and public market and ferro-contained nutrition often consumed by people, in order to identify alternative solution for handling anemia.
Methodology: True-experimental quantitative design with pre-test and post-test control group was used on three treatment groups and one control group. Respondents were anemia adolescent girls with inclusive but not exclusive criteria. 40 respondents were selected using random permutated blocks. Intervention was done for 30 days with weekly assessment. Data analysis used Friedman Test, Wilcoxon Signed Rank and Multiple Linear Regression Test.
Findings: There is a significant haemoglobin difference before and after intervention on four groups. It is seen in week 1, 2, 3, and then it tends to decline. Strong, significant correlation is found in treatment with haemoglobin and defecation duration (week 4) and bowel problems (week 2, 3, 4); feeding frequency and menstruation with haemoglobin (week 1); feeding frequency and defecation duration (week 2); mineral water intake and defecation duration (week 4). Multiple linear regression analysis results in regression equation and participants’ prediction towards dependent variables. There is a positive, significant relationship between treatment (week 2, 3) and bowel problems, mineral water intake (week 4) and defecation duration.
Conclusion & significance: Dates and ferrous sulfate consumption increase higher haemoglobin level than ferrous gluconate and 7 dates. However, ferrous sulfate and ferrous gluconate consumption have negative side effects while dates and 7dates give beneficial effects. Dates and its processed products should be considered alternative solution for handling and preventing anemia.

Biography:
Naomi Yokote is a Midwife, MHs and an Associate Professor in Maternal Nursing. She has been studying about women’s experiences and care around caesarean birth. She has published a book for general woman “The Book of Caesarean Birth for Mother” (in Japanese) in 2013 and has been giving lectures at seminars and congresses. She and co-authors has been conducting Parenting Seminar at Chubu University as new approach to prevent postpartum depression.
Abstract:
- Workshop
Location: Spessart
Session Introduction
Loredana Zordan
University College London, UK
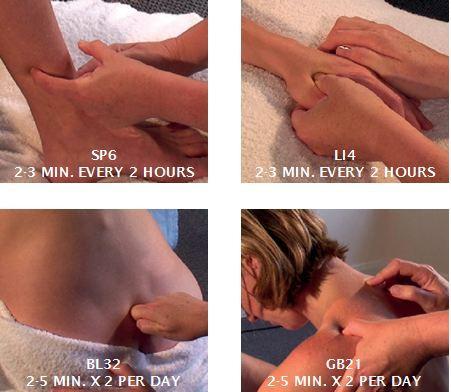
Title: Acupressure for pain relieve in labour

Biography:
Loredana Zordan is an Acupuncturist and a Midwife. She is teaching nationally and internationally by conducting workshop for midwives on the use of acupressure for pregnancy and birth. Since the introduction of the workshop in Italy “Acupressure for pregnancy and birth” many hospitals are introducing acupressure to facilitate labor induction and pain relieve in labor. This allows midwives to expand their role, becoming more complete and independent practitioner, acupressure being drug free and therefore not having harmful teratogenic effect, provides a much safer and satisfying childbirth experience as well as facilitating a more natural and less medicalized childbirth.
Abstract:

- Midwifery | Midwifery Practice and Education | Neonatology
Location: Spessart

Chair
Soheyl Asadsangabi
Vanderbilt University Medical Center, USA
Session Introduction
Loredana Zordan
University College London, UK
Title: Acupressure for induction of labour case study

Biography:
Loredana Zordan is an Acupuncturist and a Midwife. She is teaching nationally and internationally by conducting workshop for midwives on the use of acupressure for pregnancy and birth. Since the introduction of the workshop in Italy “Acupressure for pregnancy and birth” many hospitals are introducing acupressure to facilitate labor induction and pain relieve in labor. This allows midwives to expand their role, becoming more complete and independent practitioner, acupressure being drug free and therefore not having harmful teratogenic effect, provides a much safer and satisfying childbirth experience as well as facilitating a more natural and less medicalized childbirth.
Abstract:
Introduction: Acupressure is a Chinese technique that involves the use of finger pressure on specific points along the body. It has been used to induce labor in cases of post maturity. Post maturity can pose a risk for the unborn child increasing the risk of still birth. The acupressure points commonly used for induction of labor have a very strong effect on the energy of the uterus, causing uterine activity and promoting a downward expulsion of the fetus. Oxytocin is the most common induction agent used for induction of labor. It can be very useful to induce labor, but can also cause strong contractions, that can reduce the supply of blood and oxygen to the fetus causing fetal distress and on rare occasions, rupture of the uterus.
Case Study: A 36 years old primigravida, with an uncomplicated pregnancy, booked for home birth. Hospital induction was booked for post maturity at 41.5 weeks of gestation. Three days before the medical induction was due, her Bishop score was ≤6 which indicated that cervical ripening was indicated. She started using acupressure to help establish contractions and promote cervical dilatation. Author was called after two days as she was contracting; the bishop score was greater than seven. Author also used specific points to augment labor, as she was contracting irregularly. After one hour the contractions became more regular, 3 to 4 every 10 minutes. On vaginal examination, the cervix was effaced, anterior and the os 6 cm dilated. The membranes were still in intact cephalic presentation, with station at the ischial spines. After four hours, the cervix was fully dilated and she had a spontaneous vertex delivery after one hour a male infant, was born in good condition and weighing 3.800 Kg.
Conclusion: The woman and her partner were very satisfied with their birth experience, especially as they could have the home birth they wanted. They avoid being admitted to the hospital for a medical induction of labor. Acupressure increases the chance of achieving a natural childbirth, preventing potential problems which may occur during the medical induction process.
Image
Preparation for medical induction
Ineffective contractions during labour

Elinor Jenkins
Isle of Wight NHS Trust, UK
Title: Labial trauma post birth: A Delphi study of classification and suturing requirements

Biography:
Elinor Jenkins has started her Midwifery career at Isle of Wight in 1999. She moved to New Zealand to work on a case loading midwifery post for three years in 2003. On her return to UK in 2007, she joined Portsmouth Hospitals NHS Trust, where she worked for eight years as a Staff Midwife. During this time, she became Supervisor of Midwives and Research Midwife. In 2016, she has completed her Clinical Doctorate. In 2015, she took the combined post of Clinical Lead for Research and Research Manager at Isle of Wight for two years. In 2017, she returned to Clinical Midwifery and began Postdoctoral development as a Clinical Researcher. Her research into labial suturing began in 2010, when she realised that there was a significant lack of evidence for this type of genital trauma and women were not receiving evidence based care. She conducted an audit of labial suturing in 2011 and went on to gain funding for further research in 2017.
Abstract:
Introduction & Aim: Upto 49% of women sustain labial trauma during vaginal birth. Labial trauma is currently treated by midwives and obstetricians. However, there are no universally recognised descriptions of labial trauma and minimal research evidence for suturing. This study was conducted to provide guidance for current practice.
Methods: Delphi methodology was used to establish consensus for the classification and suturing requirements of several types of labial trauma. Twenty two participants with expertise in labial/perineal trauma took part. Each round consisted of six medical drawings of types and combinations of labial trauma. Each drawing had seven questions asking the participant to describe the trauma, their suturing recommendations, rationale for suturing, method of suturing, suture material, anaesthetic and technique for administration and any other comment. Numbers of agreeing participants were shown to participants on each round.
Results: Findings showed consensus that vertical skin separation of the interior aspect of the labia minora with minimal trauma to underlying tissues was described as a graze and will heal spontaneously. Deeper vertical trauma with involvement of the underlying tissue was described as a tear requiring suturing to promote healing. Lateral trauma across the labia minora was also described as a tear and needs suturing for anatomical realignment and cosmetic appearance. Suturing method should be interrupted using Vicryl Rapide 3.0 or equivalent with injected local anaesthetic.
Conclusion: This study provides unique research evidence to inform an area of practice with a limited evidence base. It also indicates future research. Its strengths are the primary data from clinical experts but its transferability now needs to be established in further research.
Sevil Hakimi
Tabriz University of medical science, Iran
Title: Comparison of breast crawl between infants delivered by vaginal delivery and cesarean section

Biography:
Abstract:
Background: Exclusive breastfeeding is the single most cost-effective intervention to reduce infant mortality. Breast crawl (BC) is deemed a natural way for the baby to behave immediately after delivery. BC is the method that may help initiation of breastfeeding in the most natural way. The aim of this study is to compare successful BC between neonates born through vaginal delivery and those born through cesarean section (CS) and factors associated with a positive outcome.
Methods: Participants were mothers who delivered their babies in Alzahra Hospital in Tabriz, through cesarean or vaginal delivery. The neonate was placed on the abdomen and mother’s chest so that the baby’s toes touched on symphysis pubis of mother after vaginal delivery, before expulsion of placenta. The infant was given 60 minutes to independently reach the nipple and take at least one suck. For mothers who had cesarean delivery, the neonate was placed on the mother’s abdomen immediately after the return from recovery room (15–20 minutes after expulsion of neonates), without washing. If the mother was unable to tolerate BC for more than 10 minutes, the midwife removed the baby from the mother’s chest. The criterion of successful BC in this study was for the baby to reach the nipple and have one or two effective sucking.
Results: Data show that babies delivered through vaginal delivery had signiï¬cantly more success in BC than babies born through the cesarean delivery (88.01% versus 11.21%). Moreover, babies in the CS group used signiï¬cantly less time to achieve BC (45 versus 28 minutes).
Conclusion: There is a remarkable difference in completion and length of time used to achieve BC between infants with regard to the delivery mode. Encouraging BC in all dyads, especially in cesarean births, may unduly delay the infant’s ï¬rst breastfeed
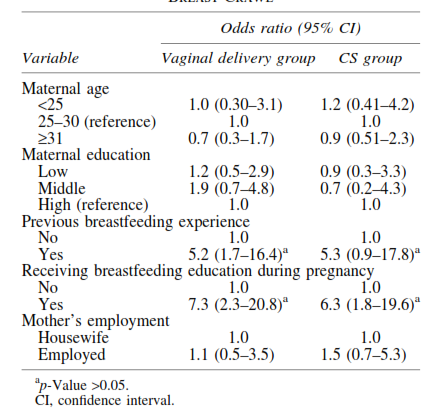
Table 1: Multivariate Analysis for Successful Breast Crawl
Indrayani
Akademi Kebidanan Bina Husada, Indonesia
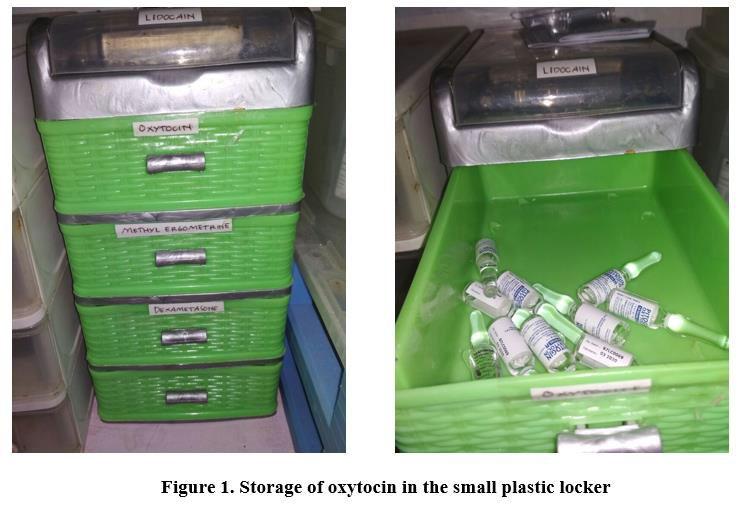
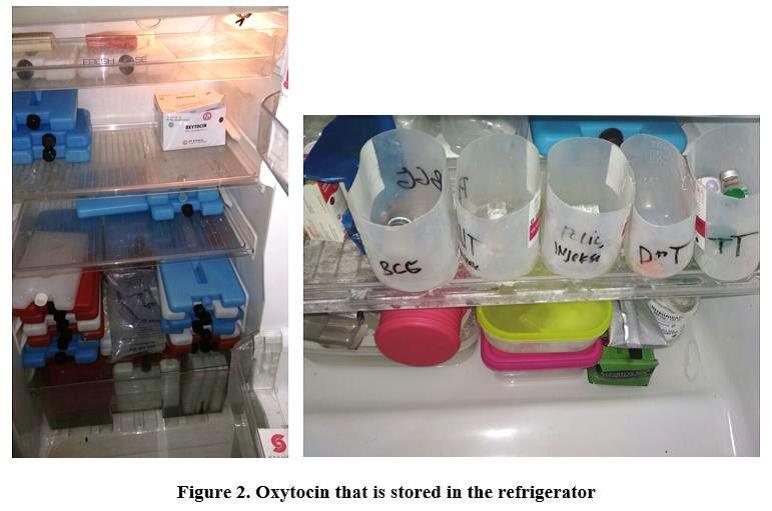
Title: How is oxytocin delivered and stored in the rural areas?

Biography:
Indrayani is a midwife with several working experiences as a nurse of public health center, midwife practitioner, midwife lecturer, researcher, and writer. Her research interests are midwives in communities, midwifery education, and maternal mortality particularly postpartum haemorrhage. Her job has led her to work with several collaborative partners such as the Ministry of Health, government and non-government institutions, association and broader community of midwives. She has published 4 books on midwifery and more than 19 papers of prosiding and journals both nationally and internationally.
Abstract:
Statement of the problem: The question is how is the delivery process and storage of oxytocin in remote areas? It is necessary to explore because oxytocin, which is an uterotonic drug, is most frequently used in low and middle income countries. International Pharmacopoeia has recommended storing oxytocin at 2-8oC and protecting it from sunlight exposure. Without cooler box, in field conditions particulary in tropical climates, oxytocin will lose its potential. This study aims to describe the delivery process and the storage of oxytocin from suppliers until it is given to patients. Methodology: A mixed method with exploratory design was used. Data collecting was done in Indragiri Hilir Regency, the Province of Riau, Indonesia. There were 32 participants getting involved in in-depth interviews and 123 respondents filled in questionaires and all were verified using supporting data. Findings: The findings of this study describe the procurement of oxytocin, the delivery process including how to carry oxytocin as well as conditions and length of storage before it is distributed or given to the patient. Conclusion & significance: The cold chain of oxytocin is not maintained from the supplier to the patient. Tolerance of the oxytocin cold chain deviation cannot be used as a justification. Given that haemorrhage is a major cause of maternal death in the world.
Tulay Kavlak
University of Istinye, Turkey
Title: Effect of non-pharmacological interventions on sleep quality in pregnancy

Biography:
Tulay Kavlak has completed her undergraduate education at GATA Nursing School in 2002; Master's degree at Gazi University in 2011 and her Doctoral degree in Gynecology and Obstetrics Nursing at Health Sciences University in 2017. Since January 2017, she has been working as an Assistant Professor in the Midwifery Department of the Faculty of Health Sciences at Ä°stinye University. Her research interests include “Postpartum period, family planning, sexual life in menopause and care after gynecological surgery”.
Abstract:
Statement of the Problem: Pregnancy is associated with significant changes in sleep architecture and pattern, which are the result of hormonal, anatomical and psychological changes occurring during pregnancy. During pregnancy, the actual incidence of sleep disturbances affecting the quality of life and well-being of women is not known. However, starting from the first trimester, it has been reported to reach the highest values in the third trimester. Aim of this study is to systematically review the literature regarding non-pharmacological interventions for improving sleep quality during pregnancy.
Methods: An electronic search strategy was conducted using several online databases (PubMed, Ovid, Science Direct, Taylor & Francis) from inception to June 2018. Inclusion criteria consisted of studies evaluating non-pharmacological interventions published in English and assessed sleep quality.
Results: 36 articles were screened and 12 studies met the inclusion criteria in the form of four prospective randomized controlled trials, two prospective quasi-randomized trials, two randomized controlled trials and four Quasi-experimental clinic trails.
Conclusion: Acupressure, sleep hygiene education, education of sleep health behavior, exercise, progressive muscle relaxation and music therapy may be associated with improved sleep quality during pregnancy. However, due to the low quality and heterogeneity of the studies yielded, a definitive recommendation cannot be made. Further higher quality research is indicated.
